Colporrhaphy
Definition
Colporrhaphy is the surgical repair of a defect in the vaginal wall, including a cystocele (when the bladder protrudes into the vagina) and a rectocele (when the rectum protrudes into the vagina).
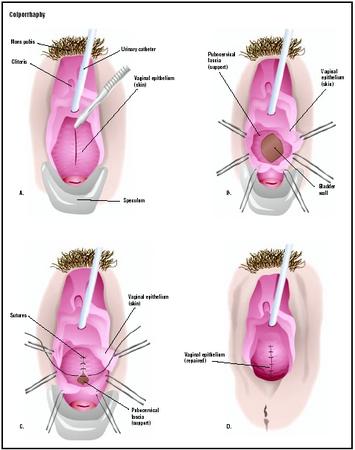
In this anterior colporrhaphy, a speculum is used to hold open the vagina, and the cystocele is visualized (A). The wall of the vagina is cut open to reveal an opening in the supporting structures, or fascia (B). The defect is closed (C), and the vaginal skin is repaired (D). (
Illustration by GGS Inc.
)
Purpose
A prolapse occurs when an organ falls or sinks out of its normal anatomical place. The pelvic organs normally have tissue (muscle, ligaments, etc.) holding them in place. Certain factors, however, may cause those tissues to weaken, leading to prolapse of the organs. A cystocele is defined as the protrusion or prolapse of the bladder into the vagina; a urethrocele is the prolapse of the urethra into the vagina. These are caused by a defect in the pubocervical fascia (fibrous tissue that separates the bladder and vagina). A rectocele occurs when the rectum prolapses into the vagina, caused by a defect in the rectovaginal fascia (fibrous tissue that separates the rectum and vagina). When a part of the small intestine prolapses into the vagina, it is called an enterocele. Uterine prolapse occurs when the uterus protrudes downward into the vagina.
Factors that are linked to pelvic organ prolapse include age, repeated childbirth, hormone deficiency, ongoing physical activity, and prior hysterectomy . Symptoms of pelvic organ prolapse include stress incontinence (inadvertent leakage of urine with physical activity), a vaginal bulge, painful sexual intercourse, back pain, and difficult urination or bowel movements.
Demographics
Approximately 50% of women report occasional urinary incontinence, with 10% reporting regular incontinence. This percentage increases with age; daily incontinence is experienced by 20% of women over the age of 75. According to a recent study, approximately 16% of women ages 45 to 55 experience mild pelvic organ prolapse, while only 3% experience prolapse severe enough to warrant surgical repair.
Description
Colporrhaphy may be performed on the anterior (front) and/or posterior (back) walls of the vagina. An anterior colporrhaphy treats a cystocele or urethrocele, while a posterior colporrhaphy treats a rectocele. Surgery is generally not performed unless the symptoms of the prolapse have begun to interfere with daily life.
The patient is first given general, regional, or local anesthesia. A speculum is inserted into the vagina to hold it open during the procedure. An incision is made into the vaginal skin and the defect in the underlying fascia is identified. The vaginal skin is separated from the fascia and the defect is folded over and sutured (stitched). Any excess vaginal skin is removed and the incision is closed with stitches.
Diagnosis/Preparation
Physical examination is most often used to diagnose prolapse of the pelvic organs. A speculum is inserted into the vagina, and the patient is asked to strain or sit in an upright position. The physician then inspects the anterior, posterior, upper (apex), and side (lateral) walls of the vagina for prolapse or bulging. In some cases, a physical examination cannot sufficiently diagnose pelvic prolapse. For example, cystogram may be used to determine the extent of a cystocele; the bladder is filled by urinary catheter with contrast medium and then x-rayed.
The patient will be asked to refrain from eating or drinking after midnight on the day of the procedure. The physician may request that an enema be administered the night before the procedure if posterior colporrhaphy will be performed.
Aftercare
A Foley catheter may remain for one to two days after surgery. The patient will be given a liquid diet until normal bowel function returns. The patient will be instructed to avoid activities for several weeks that will cause strain on the surgical site, including lifting, coughing, long periods of standing, sneezing, straining with bowel movements, and sexual intercourse.
Risks
Risks of colporrhaphy include potential complications associated with anesthesia, infection, bleeding, injury to other pelvic structures, dyspareunia (painful intercourse), recurrent prolapse, and failure to correct the defect. A fistula is a rare complication of colporrhaphy in which an opening develops between the vagina and bladder or the vagina and rectum.
Normal results
A woman will usually be able to resume normal activities, including sexual intercourse, about four weeks after the procedure. After successful colporrhaphy, the symptoms associated with cystocele or rectocele will recede, although a separate procedure may be needed to treat stress incontinence. Anterior colporrhaphy is approximately 66% successful at restoring urinary continence.
Morbidity and mortality rates
There is approximately a 1% risk of serious complications associated with colporrhaphy; the procedure is generally viewed to be safe with a very low rate of overall complications.
Alternatives
Surgery is generally reserved for more severe cases of pelvic organ prolapse. Milder cases may be treated by a number of medical interventions. The physician may recommend that the patient do Kegel exercises, a series of contractions and relaxations of the muscles in the perineal area. These exercises are thought to strengthen the pelvic floor and may help prevent urinary incontinence. One study showed an decrease of 62% in the amount of urine leakage among women ages 35 to 75 who performed Kegel exercises regularly for 16 weeks.
A pessary, a device that is inserted into the vagina to help support the pelvic organs, may be recommended. Pessaries come in different shapes and sizes and must be fitted to the patient by a physician. Hormone replacement therapy may also be prescribed if the woman has gone through menopause; hormones may improve the quality of the supporting tissues in the pelvis.